Uni-Compartmental Knee Replacement
The ends of the femur (thigh bone) and the tibia (shin bone) make up the knee joint. The two are covered by cartilage which is very smooth and hence allows the bones to glide over each other during movement. The knee cap, (the patella) also forms part of the knee joint and is held in position by tendons.
Should the cartilage be damaged, such as by injury or arthritis, pain and restricted movement is experienced as the bones rub directly on each other.
In the uni-compartmental knee replacement procedure, the damaged surfaces are removed from the worn side of the knee only whilst the remainder of the knee joint is preserved. The portion of the knee that is taken out is replaced with an artificial joint which has plastic and metal components.
The goal of the surgery is to replace a painful, deformed and stiff joint with a pain-free, well-aligned and easily moving joint.
BENEFITS OF THE PROCEDURE
- Smaller Incision – as compared to the total knee replacement the procedure involves a smaller incision.
- Smaller bone removal and bone dissection – the procedure limits the amount of bone dissection and bone removal.
- Less Blood Loss – as the procedure involves minimal incision, less blood is often lost.
- Shorter Recovery time – earlier discharge when compared to a total knee replacement and quicker return to function
FACTORS THAT MAY PREVENT YOU FROM BEING CONSIDERED FOR THE PROCEDURE
- Advanced arthritis affecting more than one compartment of the knee
- Previous anterior cruciate ligament injury
Occasionally the decision to change from a uni-compartmental knee replacement to a total knee replacement is taken at the start of the procedure if either a cruciate ligament injury of gross arthritis is seen in the knee in unexpected areas.
THE PROCEDURE
The operation should last 1-2 hours using either a general or spinal anaesthetic. An incision is made over the front of the knee. The damaged portion of bone is removed using precision instruments to ensure that the minimum amount of bone possible is removed.
The uni-compartmental knee replacement implant is then temporarily inserted to “trial” the implant. This allows the surgeon to ensure that the implant is fitting perfectly prior to the final implant being inserted. Once any minor adjustments have been made to ensure optimum fit, movement and function, the final knee implant is inserted. The wound is closed using or skin clips with a dressing and circumferential bandage to cover this.
POST OPERATION
After the surgery, you are initially moved into the recovery area and once stable, you are subsequently moved back to the ward. You will have intra-venous fluids administered using a drip in the arm. Blood tests are completed the next day and depending on the results, very occasionally, a transfusion may be needed in the post-operative period. X-rays are completed the following day done to show the position of the implant.
RELIEVING PAIN
The amount of pain relief needed after the surgery vary from one person to the next. Hence a patient specific pain regimen is administered.
REHABILITATION PROGRAM
Physiotherapists often start mobilising exercises hours after surgery. Full weight may be put on the affected knee straight away; however, you will likely require additional support. Most patients are normally ready to be discharged within 1-2 days.
ADVICE FOR ADJUSTING AND RECOVERING AT HOME
After the surgery, you will feel some pain, but it is likely to be minimal as compared to the pain felt prior to the surgery. This may last from a few days to several weeks and it is important to take pain-killers as prescribed.
The swelling and bruising that is experienced usually lasts between 6 and 8 weeks but may even last up to 6 months.
2 weeks after the surgery, the skin clips (used to close the wound may be taken out). It is usually safe to bathe at this point; however, you should follow the doctor’s recommendations.
A follow up appointment is arranged approximately 6 weeks after the operation.
Activity needs to be increased gradually by walking daily and exercising. It is often recommendable to stay away from gardening, sporting or driving activities until you are cleared by the doctor to do so.
REHABILITATION PROGRAM
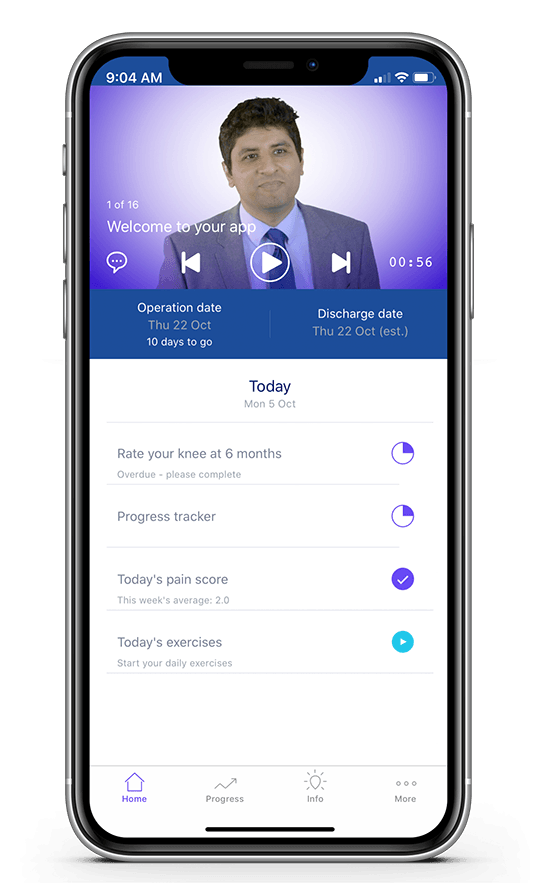
Close surveillance is advised so that possible problems are detected early and dealt with. A knee review program is used to assess how the artificial knee performs.
POTENTIAL COMPLICATIONS
In most cases, the procedure is successful. However, there are a number of risks that may be involved. Some of them are;
ANAESTHETIC
The anaesthetist will go through this with you in more detail.
INFECTION
A small risk of joint infection after the procedure exists. To prevent infections, antibiotics are usually administered during the operation. Some of the symptoms of infection include pain, swelling, redness on the wound, and even fever. Contact your doctor as soon as you detect these. There is also a small risk of chest and water work infections.
DEEP VEIN THROMBOSIS/ PULMONARY EMBOLUS
Acute pain on the calf is often a sign of blood clot in the vein. Shortness of breath/ chest pain are typical symptoms of a pulmonary embolus. Support stocking and medication to prevent these symptoms are given following the operation and need to be taken for 2 weeks post-surgery.
LOOSENING
There is the risk of the knee loosening or wearing out over time.
NEURO-VASCULAR INJURY
Damage to blood vessels or nerves can also occasionally occur following knee replacement surgery. This is rare complication but something you need to be aware of.
CONVERSION TO A TOTAL KNEE REPLACEMENT AT A LATER DATE
This occurs when the arthritis begins to progress to other areas of the knee causing debilitating symptoms.